The Economic Burden of Asthma
Asthma continues to be a major source of global economic burden in terms of both direct and indirect costs. Given that asthma cannot be cured or effectively prevented, attempts at reducing costs should focus on better disease management. This approach is consistently associated with significant reduction in asthma costs. Improving access to care, especially to controller (including preventer) therapies, and better adherence to such therapies can significantly reduce the economic burden of asthma.
Estimating the economic burden
The economic burden of a disease is the product of its prevalence; the costs due to consumable healthcare services and products such as hospital services, doctor visits, and medicines (direct costs of the disease); and costs to society, due to loss of work productivity of patients or their caregivers (indirect costs of the disease). There are challenges in estimating each of these components. For example, diagnosis of asthma may be subjective, resulting in underdiagnosis of asthma in some jurisdictions and over-diagnosis of asthma in others. Estimating direct costs is also challenging. For example, in a patient who suffers from both clinical depression and asthma, it is difficult to decide if clinical depression is because of asthma symptoms and as such should count towards costs of asthma. Robust estimation of the impact of asthma on work productivity is challenging and those that have addressed the issue mostly overlook the fact that individuals with asthma might have reduced work performance even if they attend the workplace (presenteeism).
What we know about the global costs
A recent review on the economic burden of asthma demonstrated wide variations in costs across countries. Annual direct costs varied from less than US$150 per patient (Abu Dhabi, United Arab Emirates) to more than US$3,000 per patient (United States of America (USA)), a 20-fold difference). At the national level, the total annual asthma costs in the USA increased from US$53 billion (US$60 billion*) in 2002 to US$56 billion (US$64 billion*) in 2011. Total costs of asthma for people aged 15 to 64 living in Europe were €19.3 billion (US$24.7 billion*) during 1999-2002, while in the United Kingdom alone the costs were £5 billion (US$9.8 billion*). Unfortunately, reliablenational estimates of costs are not available for the vast majority of developing countries.
In North America and Europe, asthma medicines were the largest component of direct medical costs. On the other hand, in the Middle East and Southeast Asia, outpatient costs, doctor visits, and visits to Emergency Departments were responsible for a greater proportion of the total costs. Cost estimates often ignore indirect costs but studies reporting indirect costs of asthma consistently demonstrate that these costs constitute a significant aspect of the economic burden.
The importance of symptom control
Currently, asthma cannot be cured, and there are very limited evidence-based options to prevent its development. The emphasis is therefore on achieving asthma symptom control and preventing future asthma attacks. The reduction in the costs of asthma when an individual moves from uncontrolled to controlled symptoms can be considered as a ‘preventable’ source of costs. Patients´ ability to work more productively and better cope with daily life reflects improved clinical management of their asthma. A Canadian study demonstrated that a patient with uncontrolled asthma would avoid CAD$7,768 (US$7,923*) per year in productivity loss if the disease was optimally controlled. Severe, uncontrolled asthma accounts for a disproportionately high burden in high-income countries and the availability of expensive biological therapies may add to these costs. Careful targeting of expensive novel drugs to patients expected to benefit the most from them will ensure value for money.
The role of national strategies
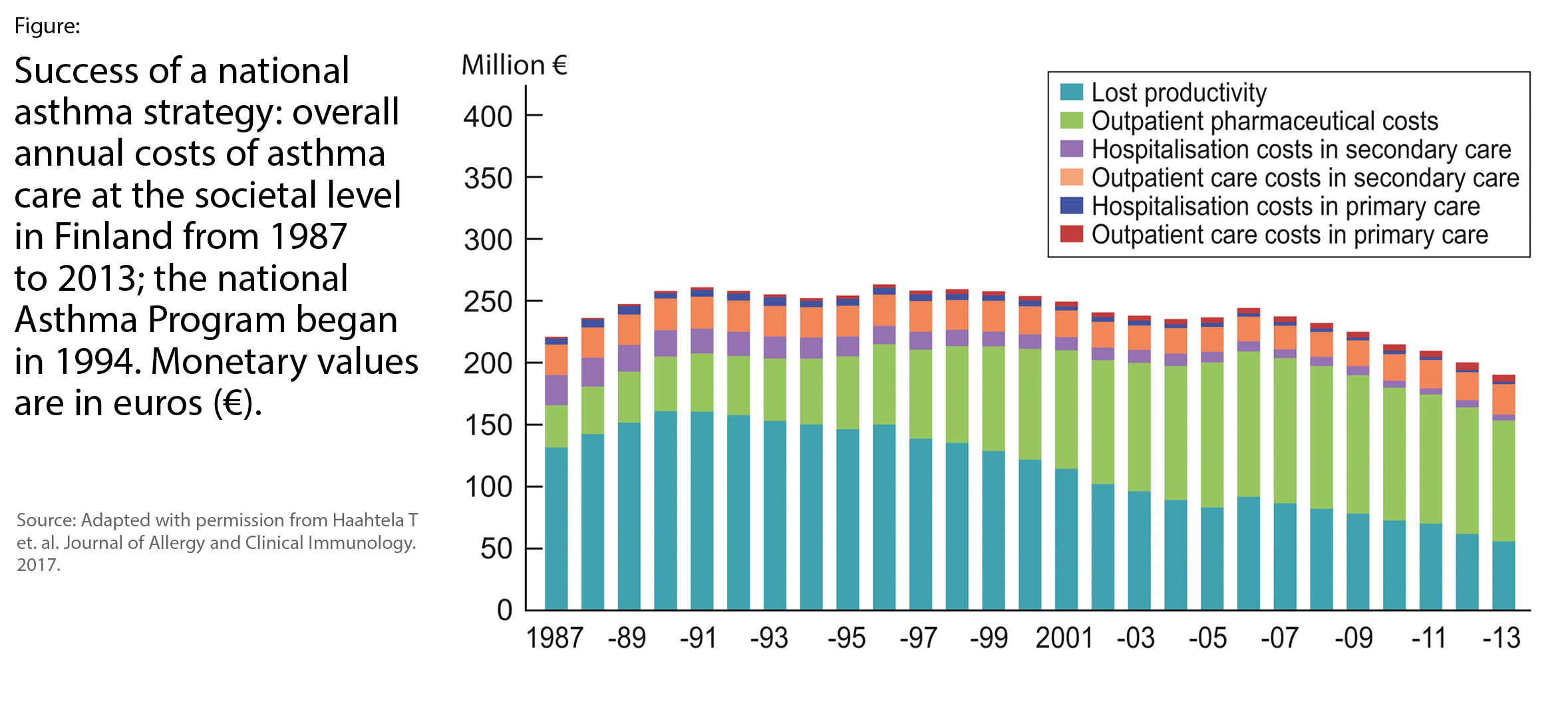
Evidence suggests that coordinated national strategies to implement changes in healthcare systems are more likely to succeed than isolated attempts at a local level. Development and implementation of national and regional asthma strategies can improve evidence-informed disease management among healthcare providers and use of medicines among patients. In Finland, with a population of 5.5 million, asthma costs have been monitored for an extended period. A nationwide Asthma Program (1994-2004) and an Allergy Program (2008-2018) have been implemented to improve asthma management across the country. From 1987 to 2013 the total annual asthma related costs decreased by 14%, from €222 million (US$249 million*) to €191 million (US$214 million*) (Figure). This overall reduction was despite a 3-fold increase in the number of patients taking medication regularly and a modest increase in asthma prevalence. Annual costs per patient also significantly decreased from €2,656 (US$2,976*) to €749 (US$839*) (72% decline).
Conclusion
Over 330 million individuals in the world have asthma, with future increases expected. Not only is the prevalence of asthma is increasing, but per-patient costs also appear to be on the rise. Developing countries are facing an even steeper increase in the future burden of asthma, and patients often do not have reliable access to the essential asthma medicines (Chapter 10). There is strong evidence that in the vast majority of patients, effective asthma control, with accessible and inexpensive preventer and controller therapies is achievable. These medicines should be part of strategies to deliver Universal Healthcare Coverage. More than ever, countries across the globe need coordinated national strategies towards both better measurement of the true burden of asthma and improving access to care and adherence to evidence-informed asthma management strategies.